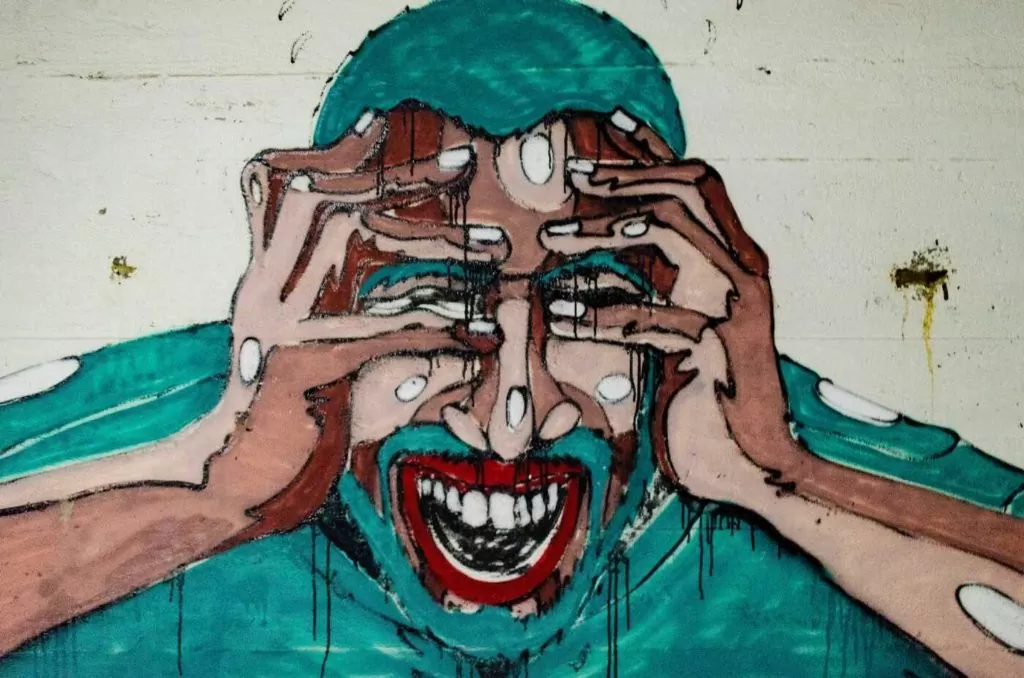
As if it weren’t bad enough to have frequent migraines, on top of a head-splitting headache you now also feel dizzy and disoriented. You can’t wait out the dizziness because your migraine is making things worse. And you can’t find a way to work through your migraine because your spinning head leaves you locked in one place.
This is a reality for people with vestibular migraine (VM). It’s no wonder that VM patients often feel that their life is defined by their condition. However, that is before they get the proper help.
Migraines are a seriously debilitating condition that
affects more Americans than diabetes and asthma combined.
And while more and more of the general population are beginning to understand that migraine attacks are far more than a simple headache solved with Advil, vestibular migraines are still unknown to the general population even though an
estimated 1% of people will get VM.
What is Vestibular Migraine?
A vestibular migraine is a nervous system problem that causes repeated dizziness (or vertigo) in people who have a history of migraine symptoms. Unlike traditional migraines, you may not always have a headache during an episode of VM.
There are many names for this type of problem. Your doctor might also call it Migraine-Associated Vertigo, Migrainous Vertigo, or Migraine-Related Vestibulopathy.
- About 30% of patients have episodes lasting minutes
- 30% have attacks for hours
- 30% have attacks over several days
- 10% have attacks lasting seconds only, which tend to occur repeatedly during head motion, visual stimulation, or after changes of head position
Following an episode, though, there is an “aftershock” period of recovery. There are patients who may take 4 weeks to recover fully from an episode. This lingering period of recovery can be the most frustrating part of VM.
- An increase in fatigue throughout the day
- Weather
- Food
- Stress
Vestibular Migraine Symptoms
- Issues with balance: feeling like your balance is off or wobbly
- Dizziness when the head is moved: a sense of spinning or dizziness during head motion. Can occur with or without nausea.
- Internal Vertigo: the false sensation that your body is rotating, twirling, swaying, or wobbling
- External Vertigo: the false sensation that the world around you is spinning or flowing
- Hypersensitive to physical movement: especially intolerant to movement of the head and neck. Changing head position brings on feelings of dizziness.
- Hypersensitive to visual movement: highly sensitive to viewing something move, possibly coming down with a sense of seasickness after witnessing movement
- Motion sickness: higher likelihood of experiencing motion sickness
- Nausea and/or vomiting: migraine-induced nausea and vomiting are associated with migraine-related vertigo
- Ear pressure: a fullness feeling in ears
You might be wondering, “With so many symptoms, how can doctors possibly diagnose VM?”
VM Diagnosis
Understanding your history and your type of dizziness is the most important part of making an accurate diagnosis. When did it start? What type of movement is it? Do you spin? Is it more of swaying or rocking? How about lightheadedness or nausea? What makes your symptoms better? What makes them worse?
It is important to organize yourself before visiting a doctor by keeping a journal of daily symptoms. There are some really good apps like Migraine Buddy and migraine journals available on Amazon to help.
Accurately describing your symptoms is vital for collaborating with your physician and treatment team. Your journal will help us look for patterns in your symptoms and then use diagnostic equipment to exclude alternative diagnoses.
Treatment Technology
Thanks to remarkable advances in science and technology, there are tests that are now involved to rule out other causes of dizziness. Your physician will typically order imaging to include an MRI and a comprehensive vestibular assessment.
Some of the diagnostic tests for vestibular disorders include:
- Videonystagmography (VNG test) – a video camera inside goggles records the eye movements in response to tests.
- Rotary Chair Test – this chair moves around to encourage responses that are on the same speed one would encounter in everyday life. It can be useful to determine if vestibular loss is occurring in both ears.
- Computerized Dynamic Posturography and Sensory Organization Tests – helps track how much you sway under different conditions. This test can show how well one adapts to unexpected movements and is beneficial in conjunction with other vestibular tests.
- VEMP – this test is performed to show if the saccule and the vestibular nerve are working properly. Small electrodes are applied to the neck and they measure the sternocleidomastoid muscle, which can show if the saccule is sensitive to sound (as it should be). Those with vestibular loss will have a low or non-existent response to noises played. This can be due to ototoxicity, Meniere’s, SCDS, or vestibular neuritis.
- Video Head Impulse Testing – this test is used to see how the eyes and inner ears work together. Small goggles with a camera record eye movements with really quick and small head movements.
Take caution, non-specialists frequently misdiagnose vestibular migraine for other vestibular disorders, such as Meniere’s Disease or BPPV. But a
Vestibular Audiologist knows what to look for and how to differentiate vestibular migraine from other conditions.
VM Treatment Puzzle
Like so many vestibular disorders, you should find solace in knowing that most people find a way to live a normal life again. They learn what works for them and move through.
Vestibular Migraine treatment consists of a combination of dietary changes, supplements, exercise, VRT (vestibular rehabilitation therapy), CBT (cognitive behavioral therapy), and medications.
Diet
This is almost always the first form of treatment because it is the “lowest hanging fruit” to grab. Working with a registered dietitian to get food sensitivity testing is an effective first start. Many patients have followed the
Heal Your Headache diet focusing on cutting out processed meats, cheeses, nuts in addition to limiting caffeine, alcohol consumption, chemical compounds, and additives.
The Dizzy Cook is a good first step resource for VM diet advice. But of course, consult your doctor to work through a proper regimen.
Supplements
Similarly, migraine patients find relief from supplements. There are several vitamins and nutritional supplements that have literature supporting their use in the prevention of migraines. Migraine patients often have magnesium deficiencies. Vitamin D, Coenzyme Q10, and Riboflavin (Vitamin B2) are all also on that list.
Vestibular Rehabilitation Therapy
Vestibular rehab therapy is the process of teaching the brain to compensate for a less efficient vestibular system. Essentially, we’re training your brain to recalibrate and find balance shortcuts that don’t put you in the same position you were before. Think of it this way: your brain is a muscle and we have to strengthen it.
VRT consists of a combination of balance training, habituation (building new habits), canalith repositioning, and gaze stabilization.
Often times, VRT sessions can elevate symptoms because you’re working through triggers and pain points in order to strengthen your balance centers. If the therapist doesn’t know what they’re doing then this program can be counterproductive by overworking a patient.
Doctors who know what they’re doing (like us), know that proper VRT ensures that the patient is always coming back to their baseline after each session to ensure that they’re not sending a patient home worse than they were prior to the therapy.
CBT (cognitive behavioral therapy)
The physical, mental, and emotional pressures that vestibular migraine bring can be demoralizing to a person’s self-esteem and outlook on life. The purpose, therefore, of CBT is to help patients elevate their mood and presence in life. It’s a means strengthening one’s mental fortitude to conquer any emotional side effects that this condition brings.
Through mindfulness, therapy sessions, and awareness, CBT trains people to build their joy and peace from the inside out.
What Now?
Overall, the outlook for people with vestibular migraine is on the rise. Research is on the rise.
Helplessness is no longer an automatic association with VM.
If you or someone you know experiences VM or thinks they do, then give us a call at (310) 954-2207 or
schedule an appointment here.